
Good Samaritan Hospital, a 300 bed acute care hospital located in Lebanon, PA was facing an over crowded emergency department (ED) but was determined to reduce wait times and improve patient flow throughout its facility. Good Samaritan embarked on an initial strategy of implementing best practices in the ED. The ED team selected the recommendations cited in the Health Care Advisory Board's Clockwork ED. To the dismay of the team, implementing best practices did not produce meaningful reductions in patient wait times. Good Samaritan's second strategy involved a year long physical expansion and redesign of the emergency department facility. The expanded ED tripled the number of available exam rooms and included new patient tracking software to improve patient flow.
In spite of the capital investment in the facility, old work patterns and procedures prevented Good Samaritan from realizing the full potential of their new building and achieving meaningful gains in performance. Good Samaritan then recruited the services of one of the country's leading consulting companies to develop a comprehensive plan and redesign ED workflow to optimize the layout of the new facility. For more than six months the consultants observed, interviewed and analyzed the performance of the ED to create an extensive report containing more than 150 recommended changes. Upon the consultant's presentation of the recommendations, the ED staff rejected the majority of the findings in the report and further progress was stalled.
Good Samaritan Hospital, with the support of Caldwell Butler (CBA), recently completed a highly successful 100 Day Quality Workout focused on “Quality Waste Recovery”. During this first 100 Day Workout, Good Samaritan’s staff identified potential gains of $6.4 million and implemented $4.3 million in tangible recovery for quality waste recuperation. Savings were tracked and validated by their finance department through the use of EXCELerator™. In addition, Good Samaritan saved 39 FTEs through the redesign of hospital workflow. With the ED initiative stalled, Good Samaritan’s leadership requested that CBA design a 100 Day Workout as a means of gaining traction in the ED. CBA’s goal was to design a workout that moved staff to action. Furthermore, success would require smooth implementation and techniques for improving the acceptance of proposed changes. Good Samaritan indicated it could not afford another long in-depth analysis or false start in the ED. Senior leadership desired assurance that rapid progress was made and momentum restored to the ED.
Accepting the challenge, CBA organized the ED staff into multidisciplinary teams each assigned responsibility for improving a sub-process of the ED workflow. The entire ED team was prepared for success by participating in an educational session exposing them to proven concepts for improving workflow. Participants were provided skills in rapid cycle testing to accelerate change. Each of the work teams reviewed potential solutions and recommendations related to their assigned challenge and selected changes in work processes to be rapid cycle tested. Ultimately, each sub-team was asked to group proposed changes into three categories as follows:
Category 1: Changes contained changes or solutions with relatively high team consensus on the best solution to implement. At the Kick-Off (Day 1) each sub-team was asked to develop a 100 Day Action Plan and design a method to test its effectiveness through Rapid Cycle Testing prior to the close of the day.
Category 2: Changes included processes and procedures the team agreed needed to be changed but could not decide what alternative solutions might be best. To overcome this hurdle, sub-teams were asked to narrow the list and identify two to three solutions they agreed would be implemented using the concepts of Rapid Cycle Testing. Rather than prolonging the discussion about the possible merits and pitfalls of each solution, they were coached to take action and test each solution using Rapid Cycle Testing. This approach allowed teams to end debate and quickly test Category 1 concepts. Instead of relying on opinion and speculation, the team generated real information on the impact of potential solution without delay.
Category 3: Changes consisted of recommended changes for which there was genuine disagreement and a lack of consensus concerning the root causes of failure. Changes in Category 3 were temporarily isolated in order to allow the team to concentrate in areas where there was a higher probability of success. CBA's Lean-Six Sigma experts then developed a strategy for analyzing the workflow for subsequent 100 Day Quality Workouts.
This approach allowed Good Samaritan's staff to make rapid progress and gain traction. By the end of the first day, each team and individual team member developed a 100 Day Action Plan specifying what was to be accomplished by the 30, 60, 90 and 120 day check-ins. Each team had a list of changes to be made and a clear strategy for testing each proposed change. On a parallel path, CBA provided a Master Black Belt to provide in-depth analysis using the techniques of a Data Summit and 14-Day Longitudinal Study to develop a comprehensive understanding of the issues listed in Category 3. This allowed the team to make progress and gain success in implementation while more extensive analysis consistent with Lean-Six Sigma's DMAIC (Define-Measure-Analyze-Improve-Control) process was deployed on the more intricate issues.
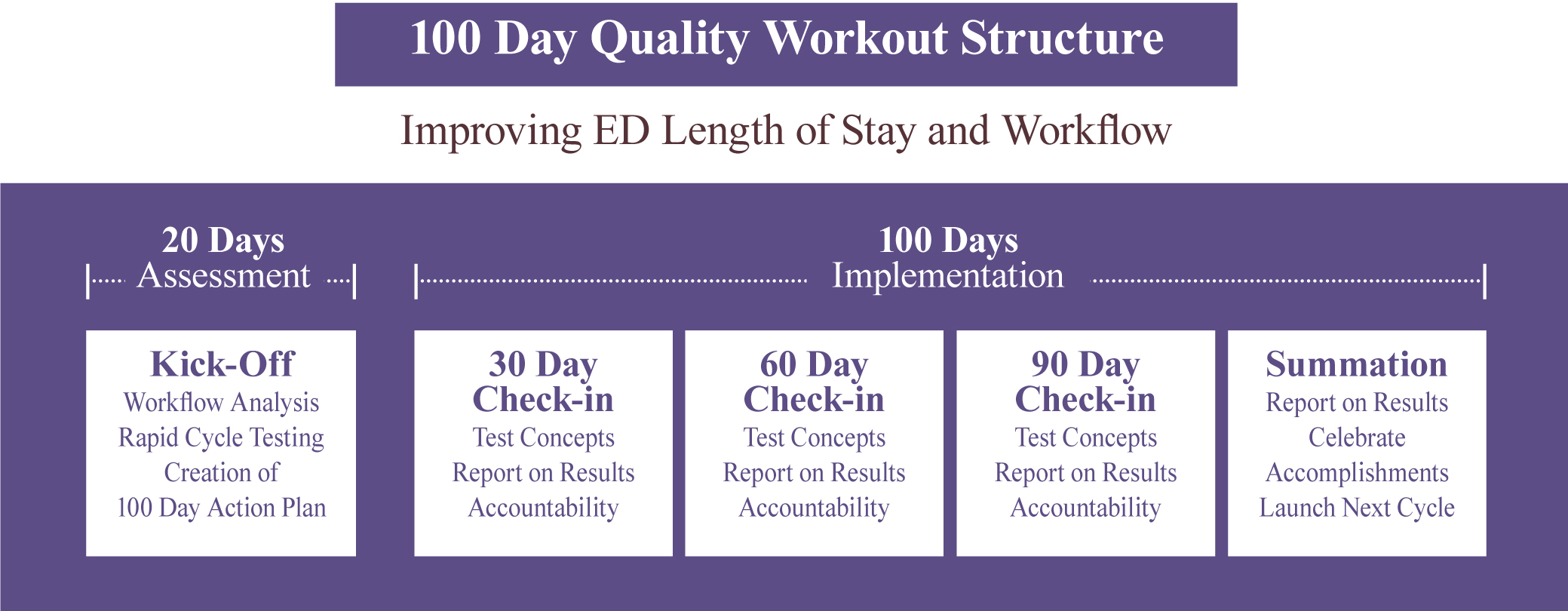
The 100 Day Quality Workout was employed as the system for driving implementation. The structure of the 100 Day Workout provided accountability and a consistent method for tracking the progress and accomplishments of each sub-team. At the Kick-Off meeting, CBA provided all the teams with training in methods for improving workflow as well as Rapid Cycle Testing. The Rapid Cycle Testing curriculum was designed to reduce the normal concerns and fears that impede change and protect the status quo. Participants were divided into sub-teams and each assigned to improve a sub-element of the ED’s work processes. After selecting improvement strategies, each team designed rapid cycle experiments to test the proposed changes. Each team had completed their 100 Day Action Plan by the end of the Kick-Off meeting. The 30, 60 and 90 day check-ins provided each team the opportunity to review their progress and discuss any issues with their peers. Each check-in allowed senior management an opportunity to monitor progress and take any corrective action necessary to ensure progress was achieved.
The ED was able to provide care without an increase in resources in spite of a 10% increase in patient volume. In the midst of this growth in demand, the teams were able to lower average length of stay by more than 20 minutes. The number of patients who left without treatment (LWBS) declined from seven per day to zero per day by the end of the first 100 Day Quality Workout, recapturing more than $1.5 million in lost revenue. The ED staff successfully Rapid Cycle Tested new protocols improving co-payments collected at the time of visit from $49.60 to $188.50 per day.